Labor
What is labor?
Labor is a
series of continuous, progressive contractions of the uterus which help the
cervix open (dilate) and to thin (efface). This lets the fetus to move through
the birth canal. Labor usually starts 2 weeks before or after the
estimated date of delivery. However, no one knows exactly what triggers the
onset of labor.
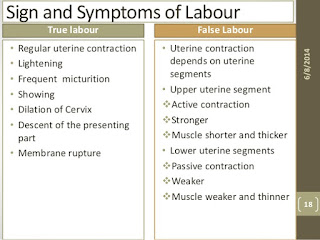
What are the signs of labor?
Signs of labor
vary from woman to woman, as each woman experiences labor differently. Some
common signs of labor may include:
·
Bloody show. A small amount of mucus,
slightly mixed with blood, may be expelled from the vagina indicating a woman
is in labor.
·
Contractions. Contractions (uterine
muscle spasms) occurring at intervals of less than 10 minutes are usually
a sign that labor has begun. Contractions may become more frequent and severe
as labor progresses.
·
Rupture of amniotic
sac (bag of waters). Labor
sometimes begins with amniotic fluid gushing or leaking from the vagina. Women
who experience a rupture of the amniotic sac should go to the hospital
immediately and contact their healthcare provider. Most women go into
labor within hours after the amniotic sac breaks. If labor still has not
begun after 24 hours, a woman may be hospitalized for labor to be induced. This
step is often taken to prevent infections and delivery complications.
If you are
unsure if labor is beginning, call your healthcare provider.
What are the different stages of labor?
Each
labor is different. However, labor typically is divided into 3 stages:
·
First stage. This is the onset of labor to complete
dilation and is divided into the latent phase and the active phase. Women
can have very strong, painful contractions during the latent phase. The
cervix dilates (opens approximately 3 or 4 centimeters) and effaces
(thins out). Some women may not recognize that they are in labor if their
contractions are mild and irregular.
·
The latent phase is
when contractions become more frequent (usually 5 to 20 minutes apart) and
somewhat stronger. This is usually the longest and least intense phase of
labor. The mother-to-be may be admitted to the hospital during this phase.
Pelvic exams are done to determine the dilatation of the cervix.
·
The active phase is
signaled by the dilatation of the cervix from 6 to 10 centimeters.
Contractions become regular, longer, more severe, and more frequent (usually 3
to 4 minutes apart). Most women feel the urge to push during this phase. In
most cases, the active phase is shorter than the latent phase.
·
Second stage. The second stage of labor starts when
the cervix is completely opened and ends with the delivery of the baby. The
second stage is often referred to as the "pushing" stage. During the
second stage, the woman becomes actively involved by pushing the baby through
the birth canal to the outside world. When the baby's head is visible at the
opening of the vagina, it is called "crowning." The second stage is
shorter than the first stage, and may take between 30 minutes to 3 hours
for a woman's first pregnancy.
·
Third stage. After the baby is delivered, the new
mother enters the third and final stage of labor--delivery of the placenta (the
organ that has nourished the baby inside of the uterus). This stage usually
lasts just a few minutes up to a half-hour. This stage involves the passage of
the placenta out of the uterus and through the vagina.
Each
labor experience is different and the amount of time in each stage will vary.
However, most women will deliver their baby within 10 hours after being
admitted into the hospital, if the labor is not induced. Labor is
generally shorter for subsequent pregnancies.
Induction of labor
In some cases,
labor has to be "induced," which is a process of stimulating labor to
begin. The reasons for induction vary. Labor induction is not done before 39
weeks of pregnancy unless there is a problem. Some common reasons for induction
include the following:
·
The mother or fetus is at risk
·
The pregnancy has continued too far past the due
date
·
The mother has preeclampsia, eclampsia, or
chronic high blood pressure
·
Diagnosis of poor growth of the fetus
Some common
techniques of induction include the following:
·
Inserting vaginal suppositories that contain
prostaglandin to stimulate contractions
·
Giving an intravenous (IV) infusion of
oxytocin (a hormone produced by the pituitary gland that stimulates
contractions) or similar drug
·
Rupturing (artificially) the amniotic sac
Care at the hospital during labor
When a woman
arrives at the hospital in labor, the nursing staff may do a physical exam
of the abdomen to determine the size and position of the fetus, and an exam of
the cervix. The nursing staff may also check the following:
·
Blood pressure
·
Weight
·
Temperature
·
Frequency and intensity of contractions
·
Fetal heart rate
·
Urine and blood samples
IV fluids are
sometimes given during labor. The IV line, a thin plastic tube inserted
into a vein (usually in the woman's forearm), can also be used to give
medicine. IV fluids are usually given once active labor has begun, and also
are needed when a woman has epidural anesthesia.
The fetus, too,
is carefully monitored during labor. A monitor may be placed over the mother's
abdomen to keep track of the fetal heart rate.
What are pain management options during labor?
A
woman has many options for pain relief that occur during labor and the
birth of her baby. Generally, mothers and their healthcare provider want to use
the safest and most effective method of pain relief for both mother and baby.
The
choice will be determined by:
·
The woman's preference
·
The woman's health
·
The health of the fetus
·
The healthcare
provider's recommendation
There
are 3 main types of pain management for labor and birth:
·
Nonmedicated measures. These measures provide
comfort and relieve stress, sometimes called natural childbirth. Many women
learn techniques to help them feel more comfortable and in control during labor
and birth. Some of these techniques include:
·
Relaxation. These techniques such as
progressive relaxation, in which various muscle groups are relaxed in series,
can help a woman detect tension and be better able to release that tension.
·
Touch. This may include massage or
light stroking to relieve tension. A jetted bath or a shower during labor may
also be effective ways to relieve pain or tension. Ask your healthcare
provider before taking a tub bath in labor.
·
Heat or cold therapy. This is used to help relax
tensed or painful areas, such as a warmed towel or a cold pack
·
Imagery. These technique of using
the mind to form mental pictures that help create relaxed feelings.
·
Meditation or focused thinking. Meditation focuses on an
object or task, such as breathing helps direct the mind away from the
discomforts.
·
Breathing. These techniques use
different patterns and types of breathing to help direct the mind away from the
discomforts.
·
Positioning and movement. Many women find changing
positions and moving around during labor helps relieve discomfort and may even
speed labor along. Rocking in a rocking chair, sitting in the "Tailor
sit" position, sitting on a special "birthing ball," walking,
and swaying may be helpful to relieve discomfort. Your healthcare provider
can help you find comfortable positions that are also safe for you and your
baby.
·
Analgesics. These are medicines to
relieve pain such as meperidine. Small amounts are generally safe during labor
and are commonly used with very few complications. However, if given in
large amounts or in repeated doses, analgesics can cause slowing of the
breathing center in the brain in mothers and babies.
·
Anesthesia. These are medicines that
cause loss of sensation include pudendal block, epidural anesthesia and
analgesia, spinal anesthesia and analgesia, and general anesthesia.
·
Local block. Anesthesia injected in the
perineal area--the area between the vagina and rectum-- numbs the area for
repair of a tear or episiotomy after delivery
·
Pudendal block. A type of local anesthesia
that is injected into the vaginal area (affecting the pudendal nerve) causing
complete numbness in the vaginal area without affecting the contractions of the
uterus. The woman can remain active in pushing the baby through the birth
canal. It is used for vaginal deliveries.
·
Epidural anesthesia (also
called an epidural block). This
anesthesia involves infusing numbing medications through a thin catheter that
has been inserted into the space that surrounds the spinal cord in the lower
back, causing loss of sensation of the lower body. Infusions of medications may
be increased or stopped as needed. This type of anesthesia is used during labor
and for vaginal and cesarean deliveries. The most common complication of
epidural anesthesia is low blood pressure in the mother. Because of this, most
woman need to have an intravenous infusion of fluids before epidural anesthesia
is given. A risk of epidural anesthesia is a postpartum headache. It may
develop if the epidural needle enters the spinal canal, rather than staying in
the space around the canal. The anesthesiologist will discuss the risks,
benefits, and alternatives to the various methods of pain relief with the
patient.
·
Epidural analgesia. This is sometimes called a
"walking" epidural because the medication infused through the
epidural is an analgesic, which relieves pain but does not numb the body and
allows movement. Combinations of medications may be used in the epidural--part
analgesic, part anesthetic. The most common complication of epidural analgesia
is low blood pressure in the mother. This type of anesthesia is used during
labor and for vaginal deliveries. A risk of epidural analgesia is a postpartum
headache. It may develop if the epidural needle enters the spinal canal, rather
than staying in the space around the canal. Epidural analgesia may be used for
pain relief in labor and for vaginal deliveries.
·
Spinal anesthesia. This type of anesthesia
involves injecting a single dose of the anesthetic agent directly into the
spinal fluid. Spinal anesthesia acts very quickly and causes complete loss of
sensation and loss of movement of the lower body. This type of anesthesia is
often used for cesarean deliveries.
·
Spinal analgesia. This involves injecting an
analgesic medication into the spinal fluid to provide pain relief without
numbing. Spinal analgesia may be used in combination with epidural anesthesia
or analgesia. This may be used during labor for pain relief or for postpartum
pain relief.
·
General anesthesia. This type of pain relief
involves giving an anesthetic agent that causes the woman to go to sleep. This
type of anesthesia may be used in emergency cesarean deliveries.


মন্তব্যসমূহ
একটি মন্তব্য পোস্ট করুন