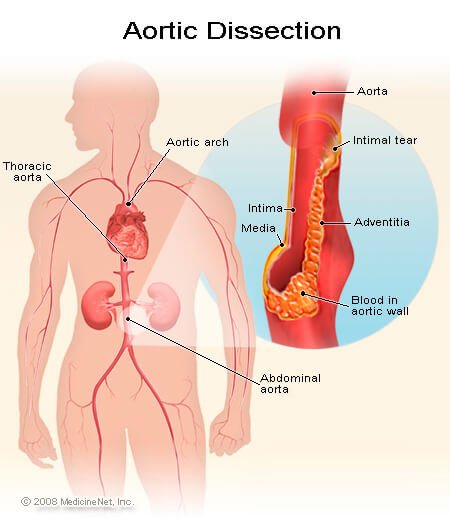
In this dramatic
condition a breach in the integrity of the aortic wall allows arterial blood to
burst into the media of the aorta. Which is then split into two layers,
creating a ‘false lumen’ alongside the existing or ‘true lumen?’
Types
(anatomical & clinical):
[A] Type-A:
·
Involves the ascending aorta.
·
Occurs in two-thirds of cases.
·
Frequently extend into the descending
aorta.
·
Peak incidence: in the 6th
& 7th decades of life.
·
H/O hypertension present in the large
majority.
·
Men are twice as frequently affected as
women.
[B] Type-B: Involves
only the descending aorta distal to the left subclavin artery.
Causes:
1.
Aortic dissection is associated with hypertension (high blood pressure) and many connective tissue disorders. Vacuities (inflammation of an artery) is rarely associated
with aortic dissection. It can also be the result of chest trauma. 72 to 80% of
individuals who present with an aortic dissection have a previous history of
hypertension.
2.
A bicuspid aortic valve (a type of congenital heart disease involving the aortic valve)
is found in 7–14% of individuals who have an aortic dissection. These
individuals are prone to dissection in the ascending aorta. The risk of
dissection in individuals with bicuspid aortic valve is not associated with the
degree of stenosis of the valve.
3.
Marfan syndrome is noted in 5–9% of individuals
who suffer from aortic dissection. In this subset, there is an increased
incidence in young individuals. Individuals with Marfan syndrome tend to have
aneurysms of the aorta and are more prone to proximal dissections of the aorta.
4.
Turner syndrome also increases the risk of
aortic dissection, by aortic root dilatation.
5.
Chest trauma leading to aortic dissection can be
divided into two groups based on etiology: blunt chest trauma (commonly seen in
car accidents)
and iatrogenic.
Iatrogenic causes include trauma during cardiac catheterization or due to an intra-aortic balloon pump.
6.
Aortic dissection may be a late sequela of cardiac surgery.
18% of individuals who present with an acute aortic dissection have a history
of open heart surgery. Individuals who have undergone aortic valve replacement
for aortic insufficiency are at particularly
high risk. This is because aortic insufficiency causes increased blood flow in
the ascending aorta. This can cause dilatation and weakening of the walls of
the ascending aorta.
7.
Syphilis will only potentially cause aortic dissection in its
tertiary stage.
Factors
that may predispose to aortic dissection:
·
Hypertension (80% of case)
·
Aortic atherosclerosis.
·
Non specific aortic aneurysm.
·
Aortic coarctation.
·
Collagen disorders: e.g. Marfan’s
syndrome.
·
Fibromuscular dysplasia.
·
Previous aortic surgery: e.g. CABG.
·
Trauma.
Clinical features:
Symptoms:
Usually acute, with very sudden onset of extremely severe pain in the chest and
back, often starting between the shoulder blades, migrating and frequently
describe as ‘tearing’
Signs:
1.
O/E there may be hypertension and
asymmetry of brachial, carotid or femoral pulses.
2.
Signs of aortic reflux (e.g. early
diastolic murmur)-in type-A dissection.
Investigations:
1.
X-ray chest P/A view: shows-
·
Broadening of the upper mediastinum (in
60%)
·
Distortion of the aorta ‘Knucke’ (in
60%).
·
Left sided pleural effusion (common).
2.
ECG: shows-
·
Left ventricular hypertrophy (in
hypertension)
·
Acute myocardial infraction (Usually
inferior)
3.
Doppler echocardiography: shows-
·
Aortic regurgitation.
·
A dilated aortic root.
·
Occasionally the flap of the dissection.
4.
Transoesophageal echocardiography
(helpful because it can only image the first 3-4 cm of the ascending aorta.
5.
CT scanning and MRI are both high
specific.
Prevention: Chronic
enlargement of the ascending aorta from aneurysm or previously unrecognized and
untreated aortic dissections is repaired electively when it reaches 6 cm
(2.4 in) in size and surgery may be recommended between for as little as
4.5 cm (1.8 in) in size if the patient has one of several connective
tissue disorders or a family history of ruptured aorta.
Management:
Initial
management comprises pain control and anti-hypertensive treatment with
labetalol to maintain the systolic pressure below 120 mm hg.
Type-A: Emergency
surgical reapir under cardiopulmonary bypass.
Type-B:
a)
Treated medically, with bed rest &
careful control of BP.
b)
Surgical intervention required if there
is evidence of leakage.
Medication
Aortic dissection generally presents as a
hypertensive emergency, and the prime consideration of medical management is
strict blood pressure control. The target blood pressure should be a mean arterial pressure (MAP) of 60 to 75 mmHg, or the lowest blood
pressure tolerated by the patient. Another factor is to reduce the shear-force
dP/dt (force of ejection of blood from the left
ventricle).
Beta blockers are first line treatment for
patients with acute and chronic aortic dissection. In acute dissection, rapidly
acting, titratable parenteral agents (such as esmolol,
propranolol,
or labetalol)
are preferred. Vasodilators such as sodium nitroprusside can be considered for
patients with ongoing hypertension, but they should never be used alone, as
they generally cause reflex tachycardia.
Calcium channel blockers can be used in
the treatment of aortic dissection, particularly if there is a contraindication
to the use of beta blockers. The calcium channel blockers typically used are verapamil
and diltiazem,
because of their combined vasodilator and negative inotropic
effects.
If the individual has refractory hypertension
(persistent hypertension on the maximum doses of three different classes of
antihypertensive agents), involvement of the renal arteries in the aortic
dissection plane should be considered.
Surgical involves:
·
Replacement of affected part with a
Dacron graft.
·
Replacement of aortic valve (sometimes
necessary).
মন্তব্যসমূহ
একটি মন্তব্য পোস্ট করুন